Clinical and Organizational Consultations
The CCE has, over its years of service, assisted with thousands of consultations. For example, in 2013 the CCE provided 607 consultations on clinical and organizational ethics issues. With this degree of activity, we are likely the most widely used ethics service in Canada. We offer 24/7 ethics service coverage.
Our clinical consultations have focused on but are not limited to the following areas:
- Brain death
- Confidentiality
- Consent and capacity
- Debriefing
- Disagreement between patients, families, and practitioners
- End of life issues
- Medical Error disclosure
- No CPR, DNR orders
- Nutrition and hydration
- Substitute decision-making
- Withdrawing and withholding life sustaining treatments
We are also routinely consulted on organizational ethics issues such as:
- Accreditation planning
- Deficit elimination plan and appeals
- Removal of medical privileges
- Resource allocation
- Role of the board in quality, ethics, risk
- Strategic planning
- Uninsured patients
- Whistle blowing
Attending Clinical Team Huddles/Unit Rounds, Notably in Teams Dealing with End-of-Life Decisions
The CCE has a great deal of expertise in aiding with end-of-life decision-making. Attendance at unit rounds/huddles serves the dual purpose of providing visibility to the clinical ethics service and its availability, and building capacity at the team level for the identification and resolution of ethics issues.
- All members of the CCE team have expertise in huddles and rounding concerning end-of-life issues.
- CCE members routinely meet with patients, families as well as teams regarding end-of-life decision-making. This is part of CCE’s proven track record of being valued members of the health care team.
Ethics Committees
We have active ethics committees, or ethics integration committees in affiliate hospitals and have experience establishing such ethics committees.
The strength of employing such a committee is that it moves beyond the “sole” bioethicist model. It is a development and improvement of the “Hub and Spokes” model by focusing on the education and development of ethics champions.
The first step in creating such committees is to identify ethics champions from across the organization and invite them to be members of these committees.
Longer-term the key tasks of Ethics Committees are to:
- Develop work plans based on the findings of the research project;
- Continue capacity building in ethical deliberation;
- Offer accreditation preparation;
- Continue policy development, revision and dissemination;
- Continue to promote and provide education.
- Support the work of the clinical ethicists at the Centre for Clinical Ethics
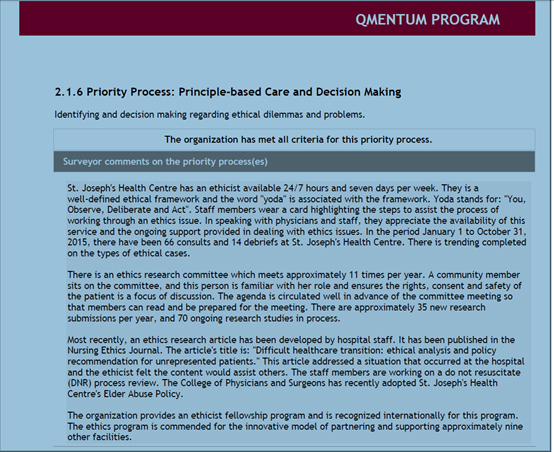
Supporting Accreditation Preparation for Accreditation Surveys
The CCE provides accreditation preparation in its yearly plans, in collaboration with the appropriate committees and key stakeholders.
The CCE has a track record of assisting hospitals to comply with accreditation standards. We have been involved in accreditation at most of the 12 healthcare organizations we provide ethics services to (over 14 years and at multiple sites).